What are Ghost Networks?
What happens when network providers do not update their information, no longer accept your insurance, are no longer practicing and you cannot seem to find anyone to see you? You get an insurance directory of ghost networks. These inaccuracies, outdated information and false data correlate to creating what is called a ghost network. When insurance companies fail to correct errors that can lead to dire consequences for people who are seeking vital mental health care and behavioral health treatment, this makes policy holders believe they have more options than are actually available to them.

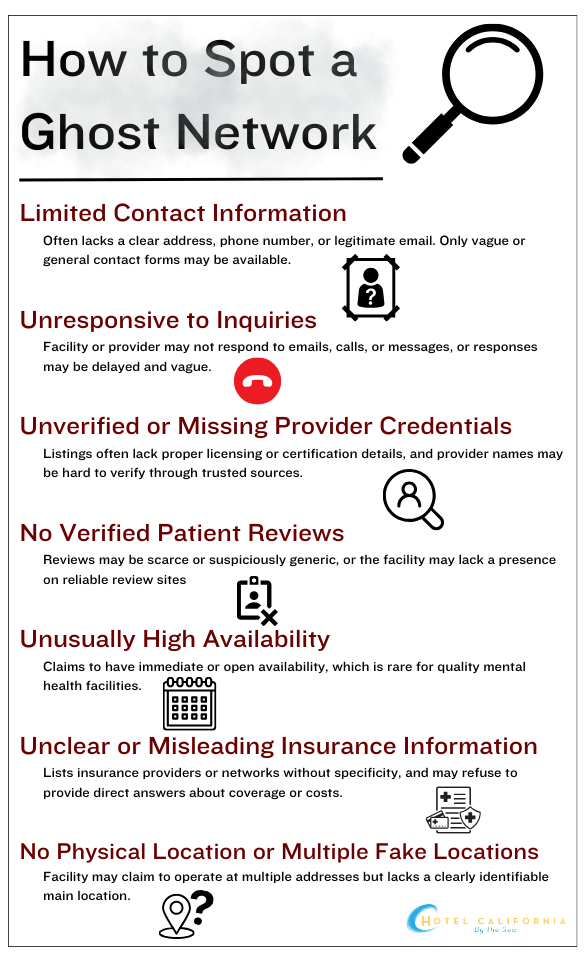
In a recent study, researchers called around 360 psychiatrists on Blue Cross Blue Shields in-network provider lists in Houston, Chicago and Boston. Some of the numbers in the directory were actually McDonalds locations and some of them were jewelry stores. And when researchers were able to reach a provider’s office, some of them no longer accepted the insurance or were not accepting new patients. The Seattle Times also conducted a similar secret shopper study of private insurance companies calling about 400 mental health providers from four of the largest insurance companies in Washington state. Only 32 of the providers on the list offered an appointment. Researchers found that the directories often had repeated listings, repeating names, providers that no longer practiced their specialty or completely incorrect phone numbers.
Ghost networks have now become a widespread problem and is now happening with many private insurances. It drives policyholders to look out of network, having to pay out-of-pocket network costs and even face delays in treatment if they get any treatment at all. In the United States alone, more than half of adults are facing mental health illness without treatment. And one significant contributor to this mental health crisis is the continued existence of ghost networks. Why are ghost networks so prevalent to begin with?
Why do Ghost Networks exist?
- Mental health care providers and behavioral health care providers listed on the insurance directory have either retired, stopped accepting that insurance or do not have up-to-date phone numbers or contact information.
- Some healthcare providers who are listed in the directory are not available to provide care as listed.
- Other inaccuracies of providers such as the wrong specialty, practice location or providers who are not accepting new patients within that network.
- Insurance companies are often slow to update and remove providers that no longer qualify from their directory. It is often not a priority because there is little incentive to do so. It is a time-consuming and often a costly maintenance upkeep leading some insurance companies to completely ignore this important task. In a 2019 report by the Council for Affordable Quality Healthcare, they found that annual administrative costs for physicians’ practices to send directory updates to insurance companies cost around 2.76 billion. On the other hand, according to the National Association of Health Insurers, insurance providers say they can’t always quickly fix errors in their network because sometimes providers fail to keep their own professional information up to date and send it to the insurers.
Factors that contribute to a Ghost Network
- Network data frequently changes as providers update their professional information. The gaps in communication between the provider and insurance company can lead to accuracy challenges and make it difficult to upkeep and verify.
- Different insurance providers have different directory requirements. Each market insurance provider has their own set of specific guidelines for accuracy requirements. This can further complicate efforts to maintain up-to-date information across organizations, which can often lead to outdated or incorrect information.
- Healthcare organizations rely on multiple data systems each serving a different purpose and used by different teams in the organization. Sometimes synchronizing provider data across all systems can be challenging and cause a delay in updated information available to policy holders.
- The rate of employee turnover and changing initiatives can also play a significant role in the prominence of ghost networks. When new people start working at the company there can be gaps in knowledge as they learn a new process. This can result in delays of important information.
Check Your Insurance Coverage for FREE
Find out if your insurance covers addiction treatment in minutes. We accept most insurance!
Cases discovering the prevalence of Ghost Networks
Healthcare giant Centene Company is one of the largest parent organizations of various healthcare-related companies. It is one of the 25 largest corporations in America and brings in more revenue than Disney, FedEx or Pepsi. However, it is much less known because its many subsidiaries use different names. It has been accused multiple times of knowingly and unknowingly presiding over ghost networks. In 2022 an Illinois insurance director fined a subsidiary of Centene more than $1 million for mental health-related violations that included providing customers with outdated provider data. Another federal lawsuit filed in Illinois found that Ambetter (a subsidiary of Centene) customers alleged that Centene company “intentionally and knowingly misrepresented” the number of available in-network providers by publishing inaccurate information.
Secret Shopper Study did their own research on provider directories and found that in May of 2023, out of 120 provider listings, an estimated 33% of the information was inaccurate, non-working or resulted in unreturned calls. Researchers were only able to make appointments about 18% of the time. They also found that more than 80% of the mental health treatment providers that were listed and attempted to contact were in fact ghosts because they were unreachable, not in-network or not accepting new patients.
How are we fighting back against Ghost Networks?
- No Surprises Act of 2021. This legislation mandates that health insurance update the information on their provider directory at least every 90 days.
- Consolidated Appropriations Act of 2023 (CAA). This legislation requires Medicaid plans to publish and update accurate searchable provider directories.
- Requiring Enhancing & Accurate Lists of Health Providers Act (REAL Health Providers Act). A bill that aims to prevent ghost networks by requiring stricter provider directory accuracy requirements for Medicare Advantage plans.
- Behavioral Health Network and Directory Improvement Act. This bill aims to address the issues of ghost networks in behavioral health care for those who are enrolled in private health insurance plans. The bill proposes stricter requirements for provider directory accuracy and calls for higher network adequacy standards. It also calls for keeping behavioral health reimbursements on par with that of physical health requirements.
- COMPLETE (Connection Our Medical Providers with Links to Expanded, Tailored and Effective) Care Act. This bill would work to increase Medicare payment rates for behavioral health integrated services. It would help with the start-up costs of implementing integrated care models and support these primary care offices during their first years with this new integrated care process.
Reach out to Hotel California by the Sea
We specialize in treating addiction and other co-occurring disorders, such as PTSD. Our Admissions specialists are available to walk you through the best options for treating your addiction.
Are you looking for Behavioral Health Treatment services?
Ghost networks greatly disrupt the healthcare system. It can be especially devastating for mental health care and behavioral health care systems because they are not often seen as a priority compared to physical health care systems. Without access to appropriate behavioral treatment services, vulnerable people across the US will continue to suffer. Ghost networks paint an inaccurate portrait of available care to consumers. These issues would be less problematic for mental health care access if insurers had up-to-date and accurate information published on their provider directories. For treatment of diseases such as substance use disorder, alcohol use disorder or co-occurring mental health disorders, a behavioral treatment program such as Hotel California by the Sea, provides a high standard of care.
We see clients at all levels of care including detox, residential, PHP and IOP. We utilize evidence-proven treatment methods such as CBT, DBT and EMDR therapy. Hotel California by the Sea is dedicated to providing the tools, resources and support clients need to overcome their addiction and reach their goals of recovery.
References:
https://questanalytics.com/news/what-are-ghost-networks
https://psychiatryonline.org/doi/full/10.1176/appi.pn.2023.07.7.10
https://blog.petrieflom.law.harvard.edu/2023/12/06/addressing-ghost-networks-in-mental-health-care/
https://www.statnews.com/2019/06/17/ghost-networks-psychiatrists-hinder-patient-care/